Cancer is the general name of a large group of diseases characterized by cells that grow out of control and have the potential to spread to other parts of the body.
Cancer cells develop when there is damage to a cell's DNA or an alteration to its functioning.
DNA is the genetic material in the cell that directs the cell's activities.
Damage to the DNA can occur for many reasons:
- Sometimes alterations to DNA that can predispose a person to getting cancer can be passed down from parent to offspring. In this case, the risk of getting cancer is inherited.
- DNA can also be damaged by external factors or things in the environment, like tobacco smoke, chemicals, viruses, and exposure to too much sunlight.
- Some cancers are thought to develop when the body's ability to deal with damaged or otherwise altered cells has been impaired by changes in hormones, metabolism, or immune conditions.
Cancer cells keep growing and dividing instead of dying and being replaced, like normal cells. Cancer cells can travel through the blood stream or the lymph system to other parts of the body and replace normal tissue. This is called metastasis.
For many cancer types, cancer cells form into a lump or mass, called a tumor. Other cancer types, like leukemia, do not form tumors, and involve the blood and blood-forming organs.
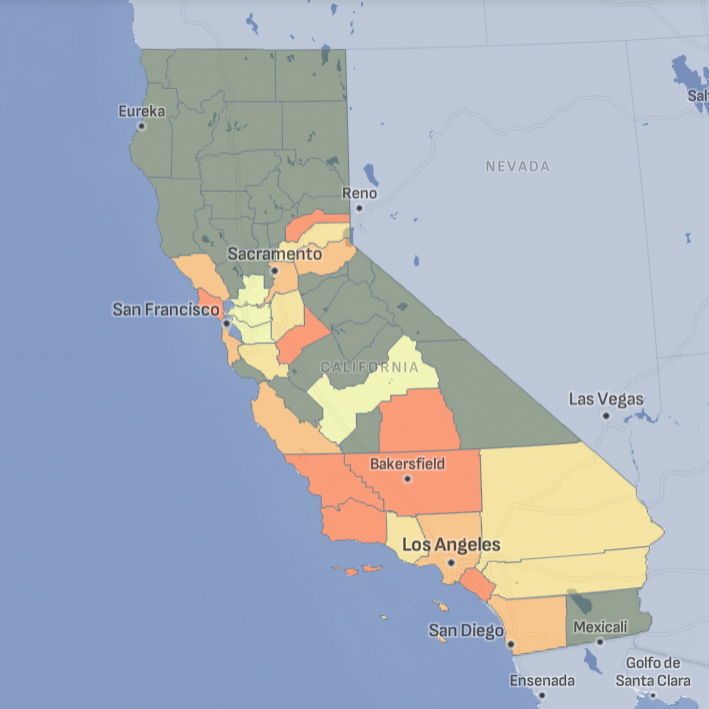
Cancer Across California
Tracking California provides data on a range of cancer types, including leukemia, lung, and pancreas, for counties across the state.
Cancer and Human Health
Cancer profoundly impacts human health by causing physical symptoms such as pain, fatigue, and weight loss, which can severely diminish quality of life. It also poses significant psychological challenges, including anxiety, depression, and emotional distress. Additionally, cancer can lead to long-term health complications, such as organ damage and an increased risk of secondary infections, due to both the disease and its treatments.
If left untreated, many forms of cancer can lead to serious illness and death. Treatment for cancer can often require invasive approaches, such as chemotherapy, although newer methods, such as immune cell therapies, are designed to be less invasive. The time frame for cancer treatment can vary widely, ranging from several months to multiple years, depending on the type and stage of cancer as well as the treatment plan. Cancer treatments often come with significant side effects, such as fatigue, nausea, and increased susceptibility to infections. In the U.S., cancer treatment can also be prohibitively expensive.
Key risk factors for cancer include:
- Diet
- Exercise
- Tobacco use
- Sunlight exposure
- Family history of cancer
- Certain viruses
- Environmental pollution
- Occupation
Although diet and tobacco use are responsible for the largest proportion of cancer cases, 35% and 30%, respectively, evidence continues to emerge suggesting that the environment plays a role in contributing to cancer.
Linking Cancer to the Environment
Cancers are a diverse collection of diseases, each with a different clinical appearance, set of symptoms, and range of severity. What they have in common is the process occurring at the cellular level that brings these diseases about.
Although this cellular process may not be the main concern among cancer patients and their families, it allows us to group cancers together, particularly when considering compounds in the environment that may be related to cancer.
All cancers are a result of a single type of cell, somewhere in the body, reproducing in a disordered way, usually at an abnormally fast pace. Knowing this helps us understand what kinds of environmental factors might be associated with cancer.
Possibilities include:
- Chemicals known to damage DNA, which contains the information cells use to reproduce normally.
- Chemicals that alter how a cell regulates its own reproduction, which may have to do with its DNA or with cellular proteins that interact with DNA.
- Chemicals that induce epigenetic modifications. Epigenetic modifications are reversible, heritable changes that impact how genes are expressed without actually changing DNA. In particular, they may play a role in cancers thought to be associated with infectious agents.
- Infectious agents (particularly viruses) that take over cellular functions and may re-arrange pieces of DNA as part of their infectious process.
- Agents that harm the immune system. A person's immune system is believed to play a role in clearing the body of at least some types of cancerous cells, so damage to the immune system may encourage some forms of cancer.
Scientists have found at least one example for each of these scenarios, but it's generally agreed that there may be others yet to be observed. Linking cancer to environmental factors is difficult as the majority of cancers take years, or even decades, to develop. Scientists rarely have the opportunity to take a large number of people, measure the amount of a specific pollutant they are exposed to, and then follow them over time to see if they develop cancer.
In its 2008-2009 report entitled Reducing Environmental Cancer Risk, the President's Cancer Panel notes that environmental sources of cancer have been largely underestimated and understudied, particularly in light of the growing incidence of a number of cancer types.
Environmental Causes and Rising Cancer Cases
Despite of how little we know, there is concern that environmental factors play a larger role in cancer than has previously been thought.
Much of this concern stems from the fact that the incidence rates of a large variety of cancers have been increasing over the last several decades. Most traditional explanations for this increase fail to explain why this is happening.
For example:
- Rates of alcohol and tobacco consumption, the behaviors most consistently linked to cancer, have been declining during the same period.
- It is unlikely that genetic susceptibility to cancer has changed at a rate rapid enough to account for the increase.
- Cancer rates have increased even among young and middle-aged people, so increased life-expectancy cannot account for the shift.
- Obesity has been increasing to alarming rates in the U.S. and abroad, and obesity may be related to some - but not all - of the cancer types for which rates have been increasing. Recent meta-analyses have linked increased body weight with esophageal cancer, thyroid, colon, and kidney cancers in men and with endometrial, gallbladder, and esophageal cancers in women.
Meanwhile, the number and quantities of compounds that could cause cancer-at least in theory-in the global environment have been increasing.
One approach used to study the role of the environment with cancer is to focus on risk factors that can be recorded or estimated, including:
Behavioral risk factors: Behaviors such as cigarette smoking or diet frequently persist over many years, so it can be relatively simple for people to quantify exposures they have experienced, even decades after the fact.
Occupational risk factors: People are frequently able to recall their work histories during the course of their lives, and in some cases records of the types and quantities of chemicals to which they may have been exposed have been kept.
Studies utilizing this approach form the foundation of much of what we do know about the environment and cancer. Learn more about specific environmental concerns and links to types of cancers here.
Who is Vulnerable to Cancer?
Anyone can get cancer, but some people are at higher risk than others. Age, sex, geographic region, race/ethnicity, and other factors can all influence your cancer risk. One way to look at disparities based on these factors is to look at the numbers of newly diagnosed cases and the numbers of deaths caused by cancer. It is important to remember, however, that many people who are diagnosed with cancer do not die of the disease.
Racial and ethnic disparities in cancer incidence and deaths
Cancer incidence, or newly diagnosed cases, and cancer deaths are not distributed equally. Some racial and ethnic groups have proportionally higher numbers of cancers and deaths from cancer than others. Higher rates of death can be because of more cases of cancer or because of more deaths among those who have the disease.
Nationally, male cancer rates are highest among Blacks, followed by Whites, Hispanics, Asian/Pacific Islanders, and American Indian/Alaska Natives. However, cancer deaths among men are higher for American Indian/Alaska Natives than among Asian/Pacific Islanders.
Nationally, female cancer rates are highest among Whites, followed by Blacks, Hispanics, Asian/Pacific Islanders, and American Indian/Alaska Natives. Cancer deaths are most common among Blacks, followed by Whites, American Indian/Alaska Natives, Hispanics, and Asian/Pacific Islanders.
No one completely understands why some groups have higher or lower rates of cancer incidence and deaths. Possible explanations include the effects of poverty and racism, environmental exposures, diet, unequal access to healthcare, unequal treatment in the health care system, and genetic factors.
Gender disparities in cancer
The most common cancers among men are prostate cancer, lung cancer, and colorectal cancer. The leading causes of cancer deaths for men are these three as well as liver cancer.
For women, the most common cancers are breast cancer, lung cancer, and colorectal cancer. These three types of cancer also account for the most cancer deaths among women.
Age disparities in cancer
People of all ages can get cancer. Some cancers are more common among children, while others are more common among older people.
For children, the most common cancers and causes of cancer deaths are leukemia and brain cancers. Most other types of cancer are more common among older populations.
Geographic disparities in cancer
Cancer is somewhat more common in some states and regions than in others. Although sometimes this can be explained by population differences (for example, a larger elderly population in one place than in another), the reasons may not be known. Possible reasons include access to health care, health behaviors like smoking, diet, and exercise, and exposure to substances in the environment that are known to cause cancer. Sometimes, it appears that a larger than expected number of people in one area have cancer. Although this may be due to random chance, it may also raise concerns about local environmental conditions that increase the risk of cancer among people in the area. Sometimes, an increase in cancer risk in a geographic area is described as a cancer cluster, although this term is inconsistently applied.
Disparities in cancer healthcare
In the United States, a patchwork of healthcare systems deliver uneven care to people across the country. Some regions, cities, and neighborhoods have access to better services than others. Within geographic areas, some people receive better care than others.
For cancer, people with good health insurance and quality medical facilities receive frequent screenings, better diagnosis, and more intensive treatment after diagnosis.
Health care access and quality is not random; in the United States, poor people and people of color are most likely to receive inadequate health care. Additionally, people of color receive less intensive care at the same medical facilities as white people.
Cancer Related Projects

Breast Cancer Mapping
This study mapped areas of California with elevated breast cancer rates based on input from community stakeholders.
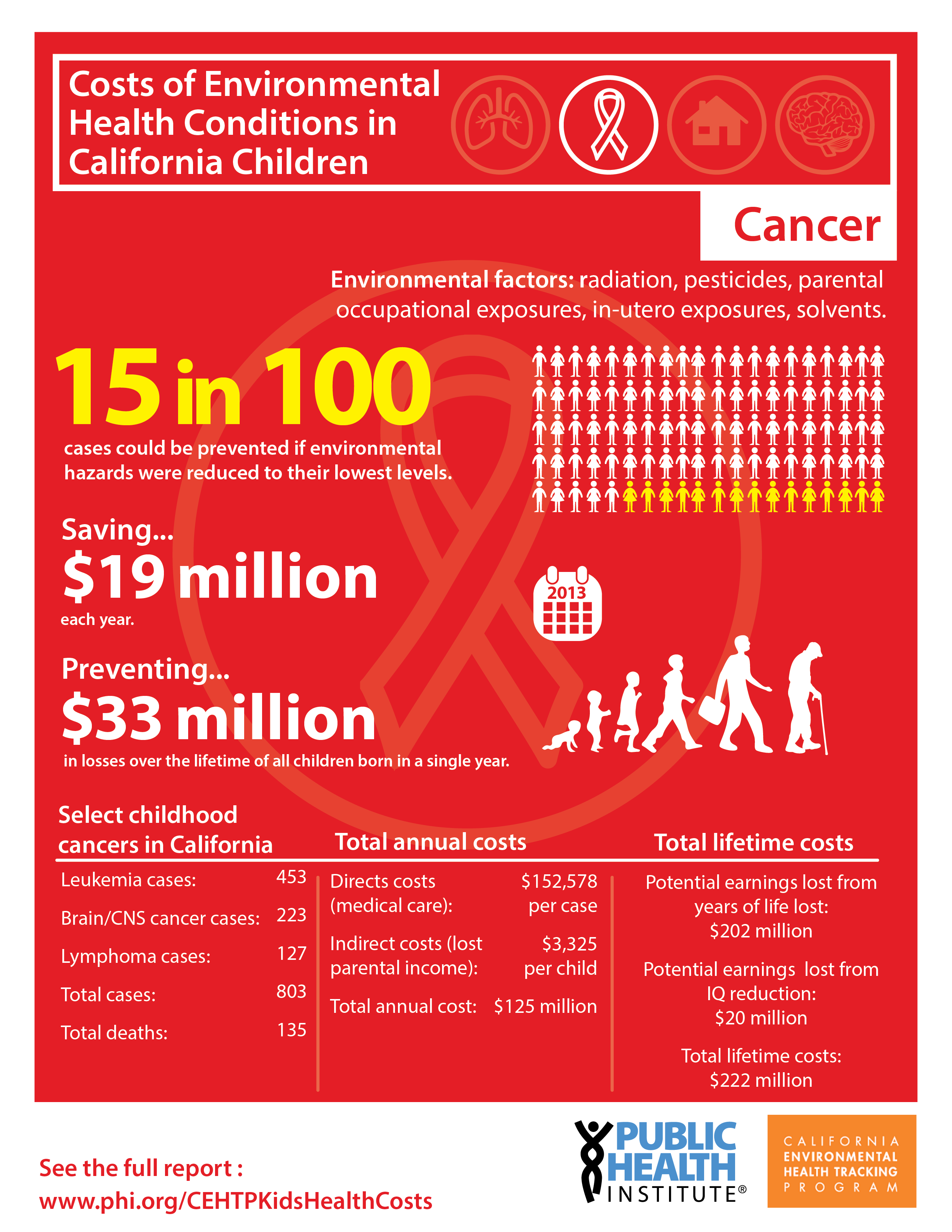
Cost of Environmental Health Conditions in California Children
An analysis of economic burden of four childhood conditions related to the environment: asthma, cancer, lead exposures, and neurobehavioral disorders.
Cancer Publications
National Trends of Bladder Cancer and Trihalomethanes in Drinking Water: A Review and Multicountry Ecological Study [2019] Cotruvo JA, Amato H
Trihalomethanes: Concentrations, Cancer Risks, and Regulations [2019] Cotruvo JA, Amato H
Estimating the Proportion of Childhood Cancer Cases and Costs Attributable to the Environment in California [2017] Nelson L, Valle J, King G, Mills PK, Richardson MJ, Roberts EM, Smith D, English P
Guidelines for the mapping of cancer registry data: results from a breast cancer expert panel study
[2013] Roberts EM, Kumar B, Collins N, Guo L, King G, Wong M, Barlow J, Bichler J, Cady L, Engel C, Garrett D, Harrison M, Morieko A, Murgai N, Tanjasiri SP, Pierce K
Prenatal Exposure to Endogenous and Exogenous Hormones and Risk of Testicular Cancer
[2006] English PB
Other Cancer Resources

California Cancer Registry (CCR)
CCR is California's statewide population-based cancer surveillance system.

National Program of Cancer Registries (NPCR)
The NPCR was established to provide funds to states and territories to improve and/or develop cancer registries.
American Cancer Society (ACS)
ACS is a nationwide, community-based voluntary health organization committed to addressing cancer through programs of research, education, patient service, advocacy, and rehabilitation.

National Cancer Institute State Cancer Profiles
NCI provides national and state-level data on cancer trends and statistics.

National Cancer Institute's Surveillance, Epidemiology, and End Results (SEER) Program
SEER collects information on cancer incidence, survival, prevalence, and mortality from specific geographic areas in the US.

