Lead poisoning is the most common environmental illness for California's children and can cause lifelong health problems, but it is preventable.
No level of lead in the body is safe, and lead can be especially harmful to the developing brain of a child. Small amounts of lead can build up in the body and cause lifelong learning and behavior problems.
Higher amounts of lead exposure can damage the nervous system, kidneys, and other major organs, and very high exposure can lead to seizures or death.
Childhood lead poisoning occurs when lead from the environment builds up in a child's body.
Young children are at greatest risk of lead exposure, and there are many sources of potential exposure for children but the most widespread is lead-based paint that was used before 1978.
Those at highest risk of lead poisoning therefore include children living in older homes, which may have peeling or chipped paint.
Communities most impacted by childhood lead poisoning include low-income families, some recent immigrant populations, and families living in older and poorly maintained rental properties.
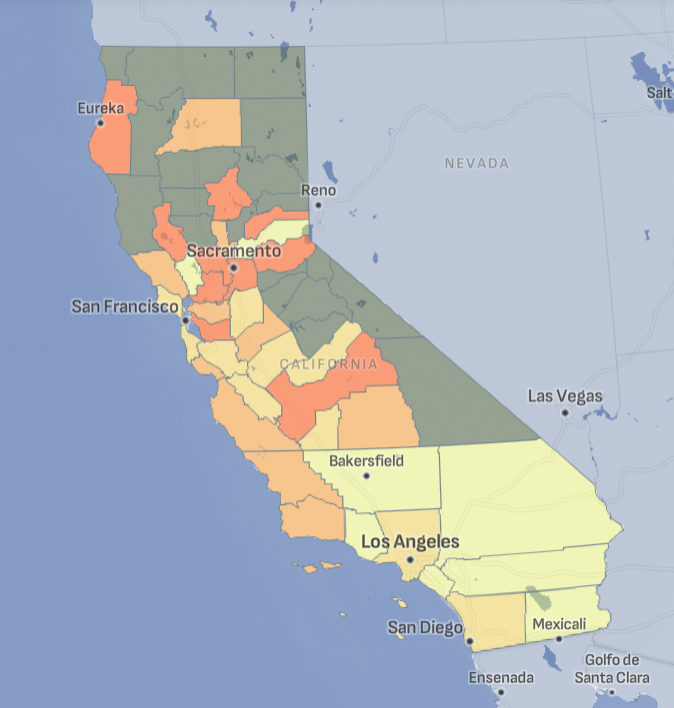
Childhood Lead Poisoning Across California
Tracking California provides data on blood lead levels for counties across the state.
Childhood Lead Poisoning and the Environment
Lead has been used for thousands of years for its durability and other qualities that made it easy to work with. Although it is a natural mineral, it is a heavy metal and is harmful to the human body even at low levels of exposure.
Children can become poisoned by lead through several common pathways:
- Ingesting lead-contaminated dust or paint chips: Older homes and buildings may have lead-based paint that deteriorates over time, creating dust and chips that children can ingest, especially during hand-to-mouth activities.
- Drinking water contaminated with lead: Lead can leach into drinking water from lead pipes, solder, or fixtures, and children who consume this water are at risk of lead poisoning.
- Exposure to contaminated soil: Soil around homes, particularly older buildings with lead-based paint or near industrial areas, can be contaminated with lead, and children may ingest or inhale this soil while playing outside.
- Using certain toys or household items: Some toys, jewelry, and household items, especially those imported from countries with less stringent regulations, can contain lead, posing a risk if children put these items in their mouths.
Historically, the greatest sources of lead exposure in the US were from leaded paint and leaded gasoline.
Lead in paint flakes off into the dust of the home and this dust can be rapidly absorbed into children's bodies. Leaded gasoline contaminates the atmosphere when it is burned, staying in the air before it settles onto the ground.
Lead in paint was banned from use in housing in 1978 and leaded gasoline was phased out in the 1990s and, as a result, levels of lead in the atmosphere dropped dramatically. However this legacy of use has left many sources of exposure in the environment, and many children are still at risk of lead poisoning through contact with lead-contaminated soil or from paint chipping or flaking in older homes.
Lead is also still regularly used in a variety of consumer products, such as some toys, candies, spices, and artisanal make-up, the use of which can put a family at risk of lead poisoning. Other potential sources of lead exposure for children include living close to sources of lead emissions, and exposure to a lead-contaminated water source.
Who is Vulnerable to Childhood Lead Poisoning?
Although people of all ages are susceptible to lead poisoning, children under six years old and fetuses are at greatest risk of harmful health effects from lead poisoning. Young children frequently crawl on floors or furniture and put their hands or other objects in their mouth, which increases the likelihood of contact with lead dust and of putting that dust into their mouths. Additionally, more of the lead that gets into their mouth is taken up into their bodies. Finally, because their brains and nervous systems are still forming, the harmful impact of lead absorption into young bodies can be greater.
In California, children with lead poisoning are more likely to come from low-income families and recent immigrant families. In large part, this is because these groups are more likely to live in older housing that is poorly maintained, so the risk of contact with lead-contaminated soil, paint or dust is higher. Additionally, some immigrant families may use imported consumer products such as cosmetics, pottery or spices that contain lead. Finally, children whose family members work in occupations that use lead or that involve contact with lead-contaminated dust are at risk of contact with the dust brought home on clothing, shoes, or equipment.
Testing for lead at 12 and 24 months is therefore recommended for the following groups because of their higher risk of lead poisoning: children in publicly funded health care, children who spend time in buildings built before 1978, and any child with a family member who works with lead.
Childhood Lead Testing
There is no single, national protocol that tells medical providers in the U.S. whom to test for lead. The Centers for Disease Control and Prevention (CDC) recommends that each state create its own guidelines for providers. Therefore, testing guidelines vary by state. Additionally, these guidelines may be difficult to find and are also rarely enforced. As a result, decisions about which children get tested for lead are often made by individual practitioners without uniform guidance.
Additionally, a blood test showing lead in a child's body can result in different responses that vary by state. Although CDC provides a reference level as guidance, there is no single blood lead level at which action is triggered, nor are these actions consistent.
Programs, policies, and funding to provide treatment for lead exposure and removal of lead hazards vary by state. Therefore, many children diagnosed with lead in their bodies do not receive meaningful assistance.
What's the difference between screening, testing, and risk assessments?
The terms lead screening and testing are often used interchangeably. They refer to the procedures where blood is withdrawn from the child and the sample is analyzed for lead.
Risk assessments are used to determine if a child should receive a lead test. The child's parents or guardian are asked questions to determine if there may be lead in the child's environment. Common questions include: Does your child live in a house built before 1978? Does your child drink or eat out of ceramic cookware? Does your child have a sibling or playmate that has been diagnosed with lead poisoning?
What are the national guidelines for children's lead testing?
The CDC recommends that decisions about lead testing be made at the state level based on local risk factors. Some states require all children be tested for lead exposure, but most states ask medical providers to conduct a risk assessment to determine whether a child should be tested for lead.
Children enrolled Medicaid are required to be tested at 12 and 24 months of age. If they are between 36 and 72 months of age and have not had a prior lead test, they are required to receive one.
What is the CDC reference level?
The reference level is the blood lead level at which the CDC recommends action be taken to remove sources of lead from a child's environment. The reference level is not a safety level. No amount of lead in the body is safe, and harm can occur at exposures beneath the reference level. However, services are generally not provided to families unless blood lead levels are much higher than the reference level.
The current reference level was determined by identifying the blood lead level at which 2.5% of children in the U.S. are estimated to be at or above, based on national survey data from NHANES. The current reference level (3.5 ug/dL) was updated in 2021.
Why might some medical providers test fewer children than others?
There are many reasons why lead testing practices vary among medical providers. These may include:
- Perception that lead is not a problem in their patient population.
- Lack of awareness of state and local guidelines.
- Limited enforcement of lead testing requirements.
- Lack of penalties for failing to test children.
Childhood Lead Poisoning Related Projects
A Hidden Problem: Lead-Poisoned Children in the U.S.
Tracking California used new analytical methods to discover that the numbers of lead-poisoned children in California and the U.S. may be much higher than previously reported.
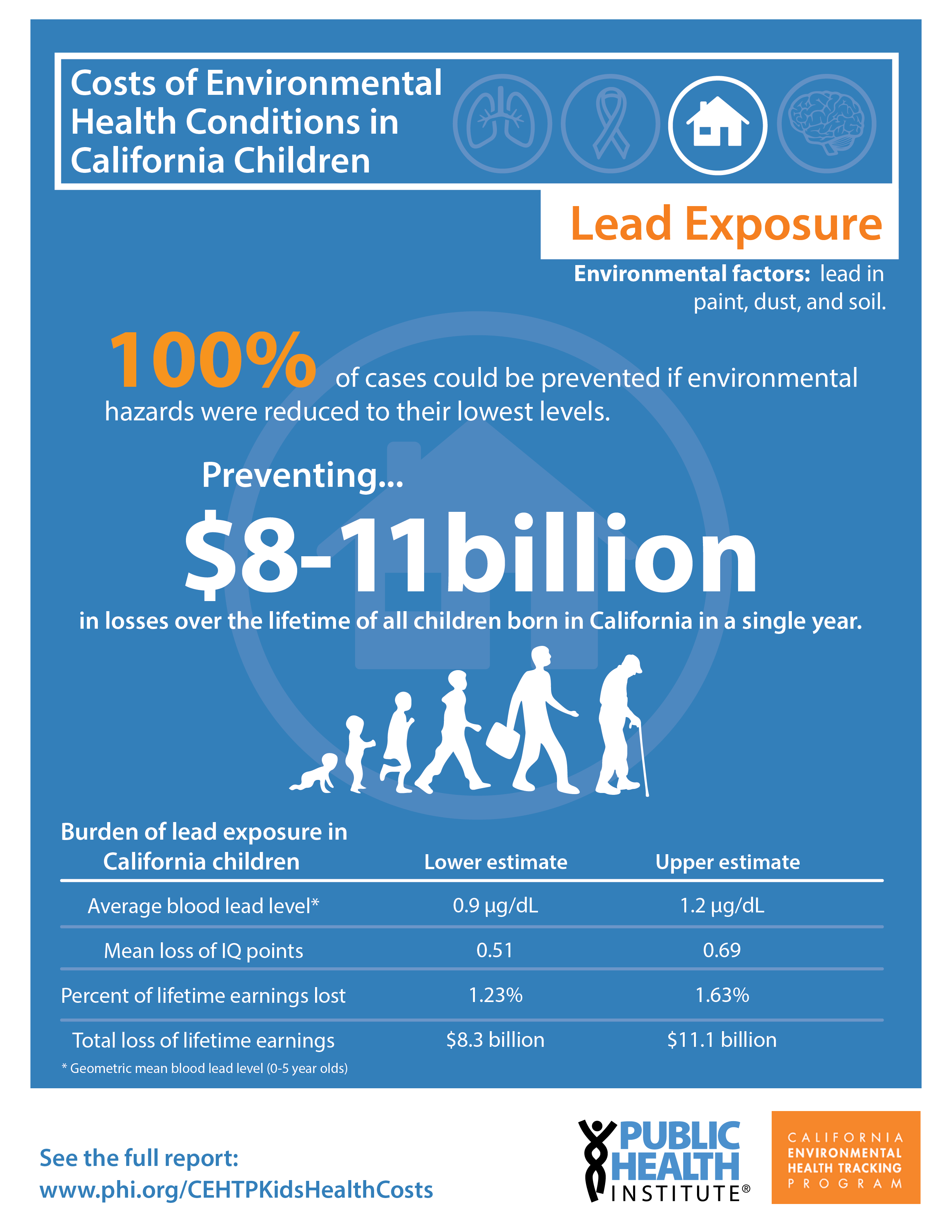
Cost of Environmental Health Conditions in California Children
Tracking California conducted an analysis to estimate the cost of four childhood conditions related to the environment in California: asthma, cancer, lead exposures, and neurobehavioral disorders.
Childhood Lead Poisoning Publications
The Consequences of Missing Children With Elevated Blood Lead Levels [2018] Madrigal D, Roberts E
Assessing Child Lead Poisoning Case Ascertainment in the US, 1999-2010 [2017] Roberts E, Madrigal D, Valle J, King G, Kite L
Analysis of multiple-variable missing-not-at-random survey data for child lead surveillance using NHANES [2016] Roberts E, English P
Other Lead Poisoning Resources

CDPH Childhood Lead Poisoning Prevention Branch
Provides resources to parents, health care providers, and other stakeholders interested in learning more about lead exposure and lead poisoning. Links to resources available in California.

CDPH Occupational Lead Poisoning Prevention Branch
Provides information for employers, workers, and others on how to prevent lead poisoning in workers.

CDC Childhood Lead Poisoning Prevention Program
Provides data, information, and resources on childhood lead poisoning at the national scale.

U.S. EPA Lead Resources
The EPA provides information on lead in paint, dust, and soil, including basic information about lead poisoning.

National Center for Healthy Housing
Provides information and resources on how to eliminate childhood lead poisoning, includes promising policies and research.
