Sickle cell disease (SCD) is a genetic disorder (a person is born with the condition, and it is not contagious) that causes normal round blood cells to become misshapen or "sickle" shaped. These sickled cells slow blood flow and that can lead to intense pain, stroke, organ damage, and other health problems.
People with SCD can live normal lives, but need specialized medical care and to take precautions to stay healthy.
One of the biggest challenges for those with SCD, especially adults, is finding and receiving knowledgeable and high-quality treatment for the disease. Staff at SCD care centers and community-based organizations can help those with the disease access quality care.
Tracking California works closely with the Centers for Disease Control and Prevention and other Sickle Cell Data Collection states to conduct public health surveillance and make the data useful to stakeholders. We use data to show how the population, health care utilization, and health outcomes for those with SCD are changing over time.
Sickle cell trait is the carrier status for SCD - it is not a disease. If both of a child's biological parents have sickle cell trait, they may have a child who has SCD.
Sickle cell trait is typically not considered a health problem; however, there is an increased risk of a rare cancer (renal medullary carcinoma) among those with trait.
Additionally, persons with sickle cell trait may have lower Hemoglobin A1c test results, which can suggest they do not have diabetes when they do.
For these reasons, it's important to know whether you have sickle cell trait (and your partner, if planning a family). The test is covered by most insurers, or if you were screened for trait at birth, your parents or doctor may know your status.
SCD Across California
Tracking California collects and provides data on those with SCD as part of a wider Sickle Cell Data Collection (SCDC) Program.

Demographics of Sickle Cell Disease in California
Black people are most likely to have SCD, but persons of any race or ethnicity can be born with the disease and about 10% of Californians with SCD are Hispanic (non-Black).
It is most frequently found in people with African, Middle Eastern, and Indian ancestry. The gene change that leads to SCD also helps people survive malaria, so it is most commonly found in areas where malaria is widespread.
Babies are born with SCD to two parents who carry the sickle cell gene either as sickle cell trait or who themselves have SCD; it is not contagious.
Before California began public health surveillance of SCD, no one knew how many people in the state lived with the disease.
As of 2021, we can see around 7,000 persons living with SCD in California, and there are probably some more than we can't see in our data (they may have private insurance and not have been in the hospital in a long time, for instance).
On average around 75-100 newborns each year are identified as having SCD through newborn screening; of these, 89% are Black/African American, 10% are Hispanic/Latino, and a small number are White, Asian, and Native American.
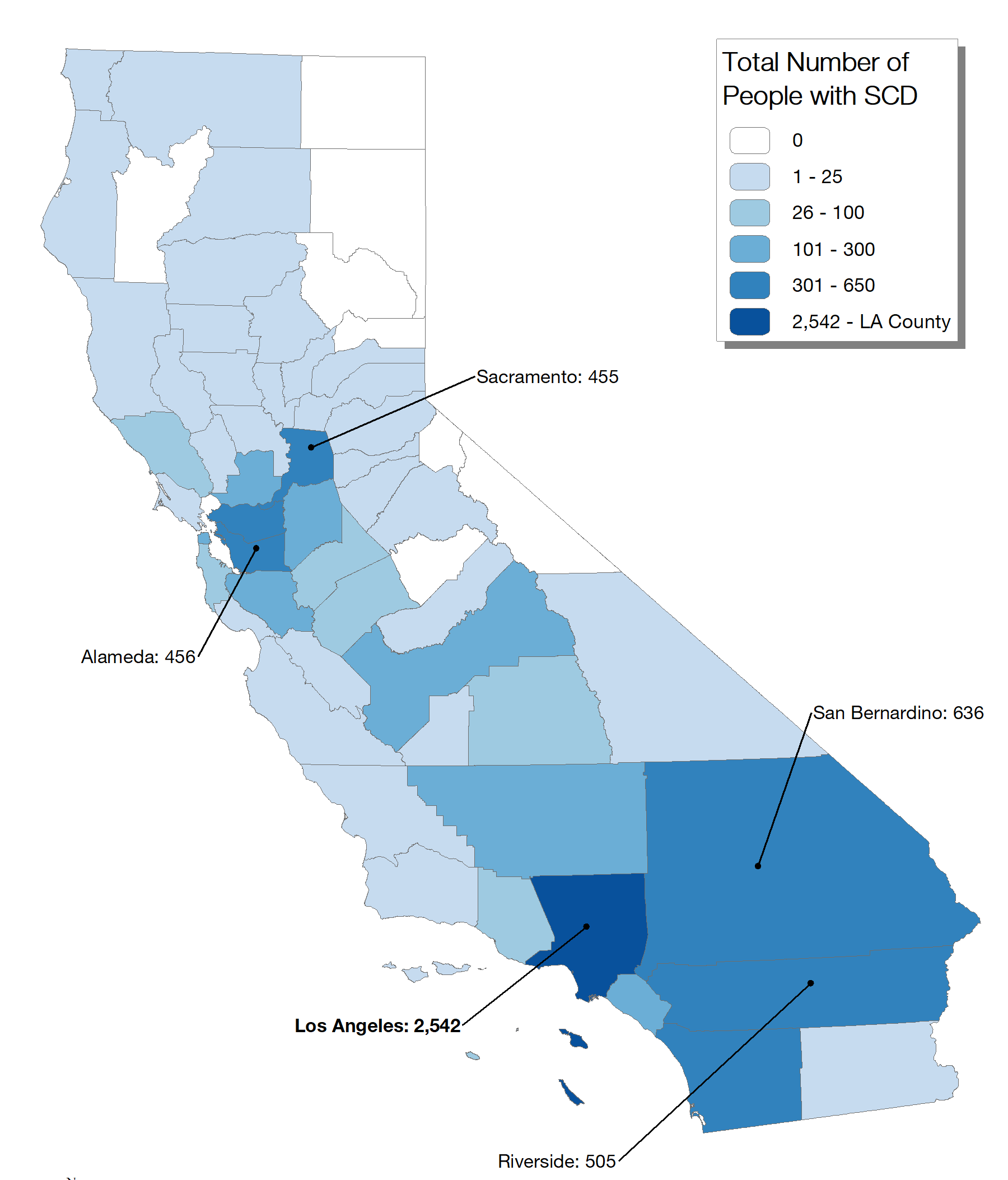
As of 2021, there is at least one person living with SCD in most counties in the state. There are people living with SCD in all urban areas (about 78% of those with SCD in California live in urban areas) and in many rural areas (22% of those with SCD live in rural areas).
Los Angeles and San Bernardino Counties have the largest number of people with SCD, while San Diego and the East Bay Area also have hundreds of people.
Here are the counties with the most people living with SCD in them in 2021:
| County | Approximate number of adults and children with SCD |
|---|---|
| Los Angeles | 2,500 |
| San Bernardino | 600 |
| Riverside | 500 |
| Alameda | 450 |
| Sacramento | 450 |
| San Diego | 350 |
| Contra Costa | 300 |
| Orange | 200 |
| San Joaquin | 200 |
Each of these counties has one or more community-based or support organizations, and most have a nearby center of high-quality clinical care for those with SCD.
Between 75 and 100 newborns are diagnosed with sickle cell disease at birth. About 3,500 newborns carry sickle cell trait. About 10% of births with sickle cell disease are Hispanic non Black, while nearly 40% of sickle cell trait identified newborns are Hispanic non Black. The rest are nearly all Black non Hispanic newborns, with a small number of White, Native American or Asian babies.
What proportion of babies born with Sicke Cell Trait in California are of Hispanic ethnicity?
The 1,500 Hispanic infants who did test positive for trait made up 37% of the 4,000 babies identified with sickle cell trait in 2010. Fewer than 1% of the ~250,000 Hispanic newborns tested that year were found to carry sickle cell trait, however. These data are provided by the state's Newborn Screening Program and the Centers for Disease Control and Prevention.
Who cares for babies and children with Sickle Cell Disease?
Children living with this disease in California usually have access to excellent care. A team of a pediatric hematologist and other specialists can work together with the child's pediatrician to provide quality health care for both sickle cell related issues and the care for health problems and preventative care that all children need. A list of pediatric care centers is here.
The Impact of Living with Sickle Cell Disease on Health
How often do Californians with Sickle Cell Disease go to the Emergency Department?
Because the complications of SCD are unpredictable, severe, and often come on at night, the emergency department (ED) is a very common place to seek medical care for persons with SCD. In particular, we found that young adults visit the ED at a high rate, perhaps because of the increase in pain episodes that begin in adolescence for many, and because adults with SCD can have a hard time getting regular, non-emergency medical care.
Who cares for adults with Sickle Cell Disease in California?
While excellent care is available for adults living with sickle cell disease in the state, it can be hard to access due to insurance issues, hours of availability, and distance/transportation.
The American Society of Hematology has a list of providers who see patients with SCD, and those transitioning from pediatric to adult care should work with their pediatric hematology team to assure a connection is made with an adult provider.
Networking California for Sickle Cell Care have expanded the network of adult clinics in the state you can find the list of adult sickle cell care clinics here.
What is the life expectancy for someone with Sickle Cell Disease in California?
Life expectancy is hard to measure because the SCD treatments and population are changing all the time. A baby born now with SCD has a very different future ahead of them than one born 20 or 30 years ago - they will have access to prophylactic penicillin as well as hydroxyurea and new treatments are being developed right now. As a result, a baby born today should have less organ damage and other complications and may therefore live a longer life.
Using our SCDC data, we can look at the age and cause of death among those with SCD in the state. When we look at older data, we see a median age of death (meaning half of people die at a younger age, half at an older age) of 45 years. But newer data reveal that the median age of death is moving upward - from 2016-2018, the median age of death is 54 years. While this is good news, the goal is that mortality among those with SCD looks the same or better than that of all Californians.
In addition, we now know more about whether death can be predicted by healthcare utilization (how often someone goes to the hospital or ED). Our findings show that it's very hard to predict, and every hospitalization or ED encounter for those with SCD should be treated as an emergency and significant health event. SCDC recently had a webinar about these findings, free for anyone to listen to.
Care and Treatment for Children and Adults with Sickle Cell Disease
 Each person with SCD should have their own plan for treatment that is developed with their health care provider.
Each person with SCD should have their own plan for treatment that is developed with their health care provider. Common parts of treatment include:
- For babies and young children, prophylactic (preventative, taken every day) penicillin to prevent bacterial infections.
- For adults and children with more severe forms of the disease, Hydroxyurea to reduce the frequency of painful episodes and other complications.
- For those who have had a stroke or other serious complications, regular ("chronic") transfusions of red blood cells (RBC) may help.
- There are several new FDA approved treatments that have shown promise is reducing the complications of SCD.
Even with the best care, some people with SCD have more severe forms of the disease and will have more health complications than others. There are new treatments being developed that may help those with severe disease.
How is Access to Medi-Cal or Other Health Insurance Related to SCD Outcomes?
One of the biggest challenges for those with the disease can be getting access to the knowledgeable healthcare providers they need to work with to stay healthy. For adult care, there are not enough hematologists and other specialists in California who are knowledgeable about SCD. People with SCD without health insurance or who live far from SCD care centers may have more health problems because of lack of quality care.
In recent years, 70% (over two-thirds) of the people with SCD we see in our data have Medi-Cal (California's Medicaid program), California Children's Services (CCS), and/or another state-run program as their only insurance or in combination with Medicare insurance.
California is a "Medicaid expansion" state, which means that under the rules of the 2014 Affordable Care Act, Medicaid insurance is available to more people than in non-expansion states. This has helped keep the number of persons with SCD and no insurance low in California. However, because Medi-Cal reimbursement rates for doctors are low, not all Medi-Cal healthcare providers are willing to take those with SCD as patients.