About people with chronic health conditions in Lake County
Chronic diseases such as asthma, diabetes, heart disease, and respiratory illnesses are widespread in Lake County. People with these conditions are especially vulnerable to climate-driven events (CDEs).
Lake County consistently reports higher-than-average rates of chronic illness compared to state and national averages. For example,
- Asthma: In 2023, Lake County’s asthma-related ED visit rate was 55 per 10,000—about 57% higher than the California average of 35 per 10,000—ranking fourth highest in the state.
- COPD: In 2023, Lake County’s emergency department visit rate for COPD was 97 per 10,000—over 3.5 times higher than the California average of 27 per 10,000, ranking second highest in the state.
- Heart attacks: Lake County's rate of emergency visits for heart attacks (34 per 10,000) was nearly 50% higher than the California average (23 per 10,000) in 2022.
- Diabetes: For the last 5 years, between 10-13% of adults have diabetes in Lake County, similar or higher to the state average of about 10%.
These health burdens are likely concentrated among older adults, low-income households, and residents with limited access to healthcare—groups already at heightened risk during climate-related emergencies.
Vulnerability to climate-driven events
People with chronic diseases are more vulnerable to the impacts of CDEs like extreme heat, wildfire and smoke, harmful algal blooms (HABs), and cold because these stressors worsen underlying health conditions, disrupt access to care, and strain already compromised bodily systems. For example:
Extreme heat
- Cardiovascular disease- Heat stresses the heart, raising risk of heart attacks and strokes.
- Respiratory conditions- Hot air and pollution worsen asthma and COPD.
- Diabetes- Heat disrupts blood sugar control and increases dehydration risk.
- Medication sensitivity- Some drugs impair sweating or temperature regulation.
- Thermoregulation issues- Chronic illness may limit the body’s ability to cool down or signal that the body is overheating.
HABs
- Liver/kidney disease- HABs toxins can damage organs when inhaled or ingested.
- Immunocompromised individuals- Higher risks from HAB exposure due to reduced immune defenses and vulnerability to pathogens and toxins in the water.
- Respiratory conditions- Airborne toxins can trigger or worsen breathing problems.
- Gastrointestinal (GI) conditions- More vulnerable to harm from contaminated water or fish.
Wildfire and smoke
- Respiratory and heart disease- Smoke worsens asthma, COPD, and heart conditions.
- Immunocompromised or cancer patients- Increased risk of lung damage and infections.
- Mobility limitations- Difficult or delayed evacuation raises safety risks.
- Treatment-dependent individuals- Disruptions to dialysis, oxygen, or meds can be dangerous.
Cross-cutting risks
- Treatment disruption- Climate events can block access to medicine, refrigerated drugs, or ongoing care.
- Electricity dependence- Power outages threaten users of oxygen, CPAPs, and mobility devices.
- Hydration/nutrition issues- Chronic illness may reduce intake during emergencies.
- Mobility and transportation barriers- Illness or disability may hinder evacuation or access to care.
Who works with this community
In Lake County, a variety of organizations support individuals living with chronic diseases, offering services ranging from medical care to educational programs and support groups. Adventist Health Clear Lake and Sutter Lakeside Hospital provide comprehensive medical care, including chronic disease management, education, and specialized services for conditions like diabetes and heart disease. The Lake County Health Services Department promotes health by focusing on an integrated healthcare and community health approach, while Lake County Behavioral Health Services provides counseling and peer support for individuals managing chronic conditions linked with mental health challenges. The Lake County Tribal Health Consortium serves Native American populations and non-Native individuals with chronic disease care, including diabetes management. Together, these organizations offer a broad spectrum of resources to help residents manage and prevent chronic diseases.
Highlights from the CHARM surveys and interviews
Selected survey findings
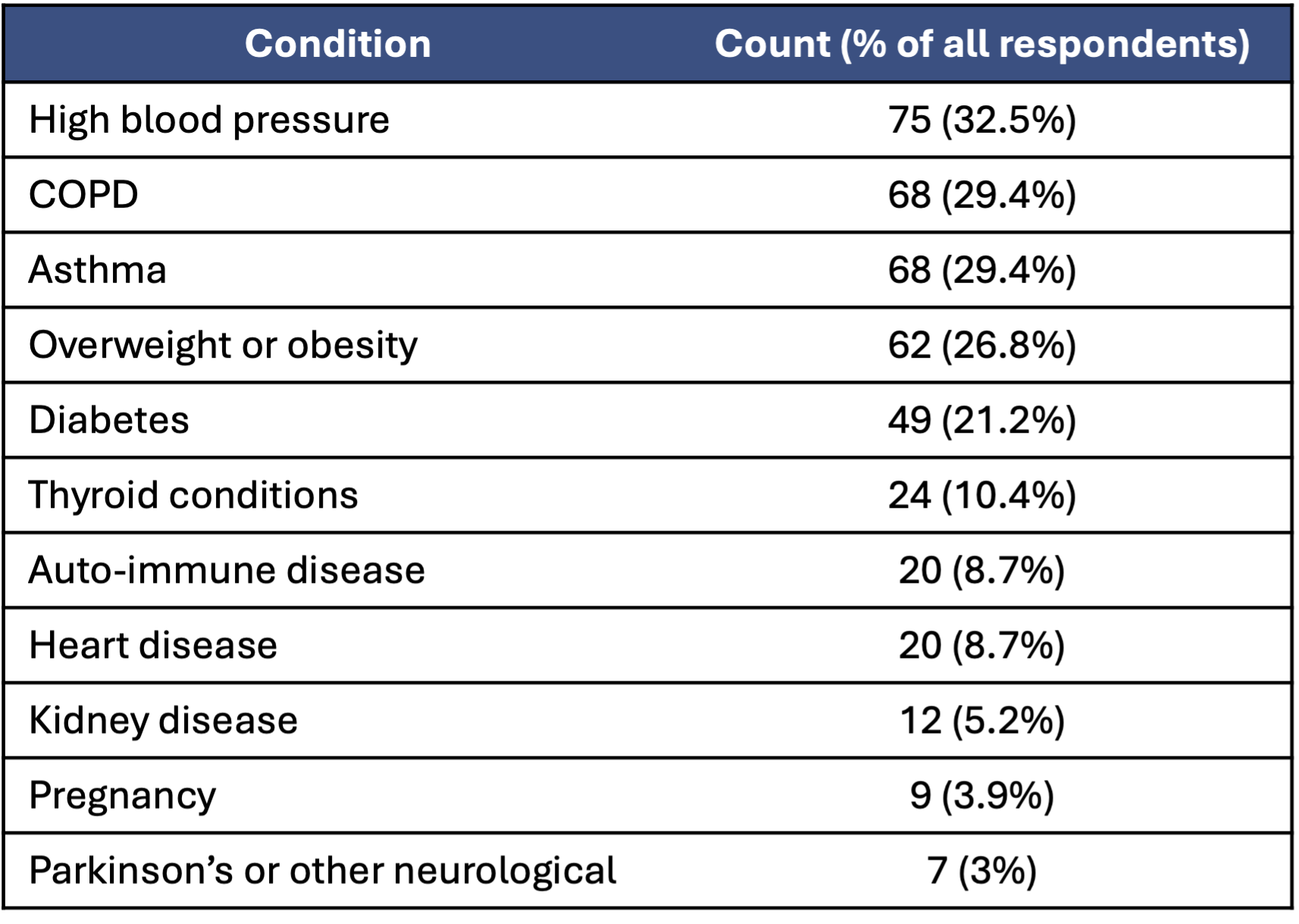
- Similar to the county as a whole, our survey respondents reported a high burden of chronic diseases. 74% of all participants identified at least one chronic health condition. The breakdown was the following:
Among those who indicated a lung-related condition (asthma or COPD):
Health was a more common concern during climate-driven emergencies: 66% reported being concerned about their health "some" or "most of the time," compared to 48% of respondents without a respiratory condition.
They reported greater support needs during Public Safety Power Shutoff (PSPS) events, particularly:
- Help making their home more comfortable in high heat (43% vs. 22%)
- An air filter or purifier (27% vs. 16%)
- A way to power medical equipment (15% vs. 5%)
- A way to keep medication cold (15% vs. 7%)
- Transportation to a hospital or to evacuate (12% vs. 6–7%)
They were more likely to take protective actions during wildfire smoke events, including:
- Staying in place (37% vs. 28%)
- Using an air filter or purifier (29%)
- Weatherizing their homes (19% vs. 12%)
- Using awnings or shade (19% vs. 12%)
Community voices
"[Participant's mother]'s physical condition is such now that she would be miserable just about anywhere...And some of her medications... are particularly critical...so my biggest fear [in an emergency] is, you know, we're going to lose touch with a medical provider."
[In response to the heat] "Absolutely... don't have the money or the gas and it's so hot outside, I have no cooling you in my car. Yeah, stresses me out. It makes my post traumatic stress, my anxiety level way up there. And then I'm depressed with it. Because I have manic depressive, a type of schizophrenia."
"Yeah, [the power outage] made me nervous, but I still use my insulin. I can't go without it. But it was for a couple days where it couldn't be refrigerated. I kept it in the fridge for as long as I could, and we had some ice packs ...and threw the insulin in with that. And it didn't last the whole time. But it the insulin, it was good enough where it didn't spoil on me or anything."
Building resilience for people with chronic health conditions
Identify and map at-risk populations
- Use health, housing, and utility data to identify individuals with chronic diseases who rely on electricity, medications, or regular care.
- Develop confidential registries or alert systems to assist during emergencies.
Strengthen communication and outreach
- Provide clear, accessible information on risks and preparedness steps tailored to people with chronic illnesses.
- Use multiple channels (SMS, phone trees, community health workers, Tribal radio) and languages to reach diverse groups.
- Engage trusted messengers- including medical providers, Tribal leaders, faith-based groups, and disability advocates- and encourage them to integrate messaging about emergency preparedness into their activities.
Ensure continuity of care
- Develop and publicize plans to maintain access to medications, dialysis, oxygen, refrigeration, and transportation during emergencies, partnering with medical care providers to ensure patients receive and understand the information.
- Partner with pharmacies, clinics, and insurers to support emergency medication supplies.
- Promote personal emergency plans (e.g., go bags with meds, contact lists, power backup options).
Enhance power backup and medical equipment support
- Distribute or subsidize backup power solutions (e.g., battery storage, solar units) for those relying on medical devices.
- Work with utilities enroll individuals in medical baseline programs to ensure priority restoration for vulnerable customers.
Improve access to resilience centers
- Expand access to resilience centers, ensuring they are accessible to people with mobility, respiratory, or sensory needs.
- Equip centers with medical support, charging stations, refrigeration, and air filtration.
Train and support community-based response
- Train community health workers, Tribal health programs, and home care providers to recognize climate risks and support clients during events.
- Conduct preparedness drills that include people with chronic conditions and their caregivers.
- Fund local resilience hubs that offer health, emergency, and social support year-round.